Understanding the Warning Signs of Spinal Narrowing
Spinal stenosis symptoms include:
- Pain or cramping in legs that improves when sitting or bending forward
- Numbness, tingling, or weakness in arms or legs
- Back or neck pain that may radiate to limbs
- Difficulty walking or maintaining balance
- In severe cases: bowel or bladder problems
Do you find yourself leaning on a shopping cart for relief while grocery shopping? Or perhaps you’ve noticed your leg pain improves when you sit down? These could be telltale signs of spinal stenosis.
Spinal stenosis occurs when the spaces within your spine narrow, putting pressure on the nerves that travel through the spinal column. It’s remarkably common – up to 95% of people show degenerative spinal changes by age 50, though many remain symptom-free.
Think of your spine as a protected highway for nerves. When that highway narrows due to bone spurs, thickened ligaments, or herniated discs, traffic jams occur – causing pain, numbness, and other symptoms that can significantly impact your daily life.
The specific symptoms you experience depend largely on where the narrowing occurs (typically in your neck or lower back) and how severe the compression has become. What makes spinal stenosis particularly tricky is that symptoms often develop gradually over time, making them easy to dismiss as “just getting older.”
Spinal stenosis symptoms vocabulary:
Top 10 Spinal Stenosis Symptoms You Shouldn’t Ignore
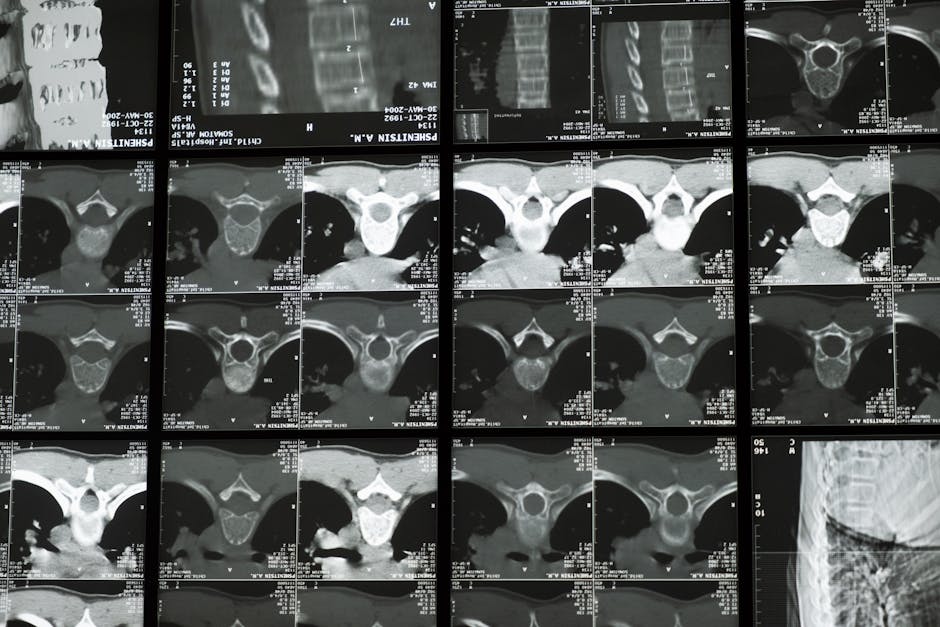
Recognizing the signs of spinal stenosis early can make a significant difference in treatment outcomes. While some people may have spinal narrowing without symptoms (as shown on imaging studies), others experience a range of discomforts that can significantly impact daily life. Let’s explore the most common warning signs that might indicate spinal stenosis.
1. Pain or Cramping Eased by Sitting or Bending Forward
One of the most distinctive spinal stenosis symptoms is pain that improves when you sit down or bend forward. This phenomenon is so common that doctors often call it the “shopping cart sign” – where patients find relief by leaning over a grocery cart while walking through stores.
“Many people describe their lumbar stenosis pain as a heavy feeling in the legs,” explains Dr. Benjamin Bjerke, a neurosurgeon specializing in spinal conditions. “What’s fascinating is how quickly symptoms can improve just by changing position.”
This happens because bending forward actually increases the space in your spinal canal, temporarily relieving pressure on compressed nerves. If you notice this pattern of relief, it’s a strong indicator of lumbar spinal stenosis.
Try this test: If walking upright causes pain in your lower back, buttocks, or legs, try walking while slightly bent forward. If symptoms improve, mention this specific pattern to your healthcare provider.
More info about back pain guide
2. Radiating Sciatica-Like Leg or Arm Pain
Spinal stenosis often causes pain that radiates along nerve pathways. In the lower back (lumbar region), this typically manifests as sciatica – sharp, shooting pain that travels from your lower back through your buttock and down your leg, sometimes all the way to your foot.
When stenosis occurs in the neck (cervical region), similar radiating pain can affect your shoulders, arms, and hands. This pain is often described as:
- Electric-like or burning sensations
- Shooting down specific pathways
- Worse with certain movements or positions
- Accompanied by tingling or numbness
As one 60-year-old patient reported: “I initially thought the tingling in my foot was just from the cold weather. It wasn’t until it persisted and started moving up my leg that I realized something more serious was happening.”
Scientific research on sciatica
3. Persistent Numbness or Tingling
Paresthesia – the medical term for abnormal sensations like numbness, tingling, or “pins and needles” – is another common symptom of nerve compression from spinal stenosis.
These sensations typically follow specific patterns based on which nerves are affected:
- Lumbar stenosis may cause numbness in the buttocks, legs, or feet
- Cervical stenosis can produce tingling in the shoulders, arms, or hands
What distinguishes stenosis-related numbness from other causes is its pattern and triggers. The numbness may:
- Begin after standing or walking for a period
- Improve with rest or position changes
- Follow specific dermatome patterns (areas of skin supplied by particular spinal nerves)
- Progress gradually over months or years
4. Muscle Weakness and Foot Drop

When spinal stenosis compresses motor nerves, muscle weakness can result. One particularly telling sign is “foot drop” – difficulty lifting the front part of your foot when walking.
“Foot drop in spinal stenosis arises from compression of specific lumbar nerve roots (L4, L5, S1) and can manifest as tripping or dragging of the foot,” notes a recent clinical review. This weakness occurs because the nerves that control the muscles lifting your foot become compressed.
Signs of foot drop include:
- A slapping sound when your foot hits the ground while walking
- Tripping frequently
- Needing to lift your knee higher than normal to clear your foot from the ground
- Dragging your toes when walking
This symptom represents more advanced nerve compression and warrants prompt medical attention to prevent permanent weakness.
5. Balance Problems or Hand Clumsiness
Spinal stenosis, particularly in the cervical spine, can affect your balance and coordination. When the spinal cord itself becomes compressed (a condition called myelopathy), signals to and from your brain become disrupted.
Signs of this more serious compression include:
- Difficulty with fine motor tasks like buttoning shirts or writing
- Unsteady walking, especially in the dark
- A feeling of heaviness or stiffness in the legs
- Frequent falls or near-falls
These symptoms indicate compression of the spinal cord rather than just nerve roots and require prompt medical evaluation.
More info about manual therapy
6. Heavy, Cramping Legs After Short Walks
A hallmark of lumbar spinal stenosis is neurogenic claudication – leg pain, cramping, or heaviness that develops after walking short distances and improves with rest. This symptom is often confused with vascular claudication (poor circulation), but there are key differences:
| Neurogenic Claudication (Stenosis) | Vascular Claudication (Circulation) |
|---|---|
| Improves with sitting or bending forward | Improves with standing still (no need to sit) |
| Walking uphill may be easier than downhill | Walking uphill is always worse |
| Can occur with standing without walking | Requires exertion to trigger symptoms |
| Position changes provide relief | Position doesn’t matter, just rest |
| Bicycle riding often comfortable | Bicycle riding may cause pain |
“Some people describe their lumbar stenosis pain as a heavy feeling in the legs,” notes a clinical report. “Others report an electric-like or burning sensation radiating down the leg.”
The distance you can walk before symptoms begin (your “claudication distance”) is an important measure of stenosis severity and can help track progression over time.
7. Dull Ache or Stiffness in Back or Neck
While the radiating symptoms of spinal stenosis often get the most attention, many patients also experience localized pain in the affected region of the spine. This can manifest as:
- Morning stiffness that improves with movement
- Dull, aching pain in the lower back or neck
- Discomfort that worsens with certain positions (especially extension/arching backward)
- Pain that improves with rest
This local pain stems from the same degenerative changes causing the stenosis – bone spurs, facet joint arthritis, and thickened ligaments. While less specific than other symptoms, this pain often accompanies the more distinctive signs of nerve compression.
8. Burning or Electric-Like Arm Pain
Cervical spinal stenosis frequently causes distinctive arm pain patterns. As one specialist describes: “Patients often report burning or shock-like pain radiating from the neck into the shoulder, arm, and sometimes into the hand.”
This pain follows specific nerve pathways depending on which level of the spine is affected:
- C5 nerve compression: Pain/numbness in the shoulder and upper arm
- C6 nerve compression: Pain/numbness in the arm and thumb/index finger
- C7 nerve compression: Pain/numbness in the middle finger
- C8 nerve compression: Pain/numbness in the ring and little fingers
Unlike musculoskeletal shoulder pain, cervical radiculopathy (nerve pain) typically:
- Radiates below the elbow
- Follows specific dermatome patterns
- May be accompanied by reflex changes
- Often worsens with neck movements
9. New Bowel or Bladder Difficulties
While rare, one of the most serious spinal stenosis symptoms is the development of bowel or bladder dysfunction. This can include:
- Difficulty initiating urination
- Incontinence (inability to control bladder or bowels)
- Decreased sensation in the “saddle” area (genitals, buttocks)
- Sexual dysfunction
These symptoms indicate a condition called cauda equina syndrome – severe compression of the nerve bundle at the base of the spine. This is considered a medical emergency requiring immediate attention.
“If you experience sudden changes in bowel or bladder function along with back pain or leg symptoms, seek emergency care immediately,” advises Dr. Louis Chang, a neurosurgeon specializing in spine disorders. “This combination of symptoms requires urgent evaluation.”
10. Sudden Paralysis or Rapidly Worsening Weakness
While spinal stenosis typically develops gradually, in rare cases it can cause sudden, severe symptoms. Rapid progression of weakness, especially if it affects both legs or arms, warrants emergency medical attention.
Warning signs that require immediate medical care include:
- Sudden inability to walk
- Rapidly progressing weakness in limbs
- Severe, sudden onset of pain
- Loss of consciousness
- Inability to urinate despite a full bladder
These symptoms may indicate severe spinal cord compression that could lead to permanent damage if not addressed promptly.
Scientific research on cauda equina
Region Matters: How Spinal Stenosis Symptoms Differ in the Neck vs. Lower Back

Your spine isn’t just one uniform column – it’s a complex structure with distinct regions, each affecting your body in unique ways when stenosis develops. Think of it like traffic congestion in different parts of a city – a jam downtown creates different problems than one in the suburbs. Let’s explore how spinal stenosis symptoms vary depending on whether the narrowing occurs in your neck or lower back.
Cervical “Spinal Stenosis Symptoms” Checklist
When the narrowing happens in your neck (cervical spine), the effects can be particularly concerning because this area houses not just nerve roots but your spinal cord itself.
The most common cervical spinal stenosis symptoms include neck pain and stiffness that typically worsens when you look up or arch backward. Many patients describe a distinctive radiating arm pain – an electric or burning sensation that travels from the neck down through the shoulders and arms, sometimes reaching the hands.
Hand function often becomes a telling sign of cervical stenosis. “I first noticed something was wrong when I couldn’t button my shirt easily,” shares one patient. This hand weakness or clumsiness with everyday tasks can be an early warning sign, along with numbness or tingling that follows specific nerve patterns in your arms and hands.
Balance problems are another red flag, especially difficulty walking in dimly lit areas. You might also experience headaches, particularly at the base of your skull, or have abnormally brisk reflexes that your doctor can detect during an examination.
As Dr. Girardi, an orthopedic surgeon, reassuringly notes: “Even if we can’t get the patient back to all the physical activities he or she once enjoyed, we can often get them back to performing activities of daily living without discomfort.”
In more advanced cases, cervical stenosis can progress to a condition called myelopathy, where the spinal cord itself is compressed. This serious development brings challenges with coordination and balance, weakness affecting both arms and legs, and sometimes even electrical sensations that shoot down your spine when you bend your neck.
More info about chronic back pain PT
Lumbar “Spinal Stenosis Symptoms” Checklist
The lower back (lumbar region) is the most common site for spinal stenosis, and its symptoms primarily affect your legs and feet rather than your arms.
The hallmark of lumbar spinal stenosis symptoms is neurogenic claudication – a fancy medical term for the pain, cramping, or heaviness in your legs that gets worse when you walk or stand but improves when you sit down. Many patients describe it as feeling like their legs are extraordinarily heavy or tire out quickly when walking.
Low back pain is often present but might be surprisingly mild compared to the leg symptoms. The classic “shopping cart sign” – where leaning forward on a cart provides relief – is a distinctive pattern that helps doctors identify lumbar stenosis.
Another telltale sign is finding it easier to walk uphill than downhill – the opposite pattern of what happens with circulation problems. This occurs because bending slightly forward while walking uphill creates more space in your spinal canal, temporarily relieving pressure on compressed nerves.
Numbness or tingling in your legs or feet often accompanies the pain. While these sensations may affect both legs, they’re frequently more intense on one side. In more advanced cases, you might develop foot drop – difficulty lifting the front part of your foot when walking, which can lead to tripping or a slapping sound when your foot hits the ground.
“One hallmark sign of lumbar spinal stenosis is decreased walking tolerance due to neurovascular compression,” explains a physical therapy resource. “Forward bending (flexion) and sitting often relieve symptoms, while extension and standing worsen them.”
Thoracic & Tandem Stenosis—The Rare but Real Culprits
While stenosis most commonly affects the neck and lower back, it can sometimes develop in less typical locations, creating unique symptom patterns.
Thoracic stenosis (mid-back) is relatively uncommon but creates distinctive symptoms when it does occur. Patients often describe a band-like pain wrapping around their chest or abdomen, almost like wearing a tight belt. Some experience unusual electrical sensations with certain movements or develop balance problems and leg weakness that can be mistaken for other conditions.
Even more complex is tandem stenosis, where narrowing occurs simultaneously in multiple spinal regions. This creates a mixed symptom pattern that can be confusing during diagnosis – you might have both arm and leg symptoms that don’t seem to follow the typical pattern of either cervical or lumbar stenosis alone.
As one specialist notes, “Spinal stenosis is most common in the lumbar and cervical spine and rarely occurs in the thoracic spine.” However, recognizing these less common presentations is crucial for getting an accurate diagnosis and appropriate treatment.
Understanding exactly where your stenosis is located helps determine the most effective treatment approach – whether that’s targeted physical therapy, medication, or in some cases, surgical intervention.
When to Seek Help: Diagnosis, Treatment & Prevention

Living with spinal stenosis symptoms doesn’t mean you have to accept pain as your new normal. Knowing when and how to seek help can make all the difference in your recovery journey.
Getting a Precise Diagnosis for “Spinal Stenosis Symptoms”
Finding the root cause of your pain typically follows three important steps:
First, your doctor will have a heart-to-heart conversation about your symptoms. They’ll want to know when your pain started, what makes it better or worse, and how it’s affecting your daily life. This detailed history helps paint the picture of what’s happening in your spine.
Next comes the hands-on detective work. During your physical exam, your doctor will check your strength, reflexes, and sensation. They might perform special tests like the Spurling’s test (gently extending and rotating your neck) or a straight-leg raise to see if these movements reproduce your symptoms. They’ll also watch how you walk and test your balance, looking for clues about which nerves might be affected.
Finally, imaging confirms what your symptoms suggest. X-rays show bone changes like spurs or narrowed spaces, while an MRI reveals the soft tissue details – showing exactly where nerves might be compressed. For some patients, a CT scan (sometimes with a special dye called a myelogram) offers detailed bone imaging, while nerve conduction studies help identify specific affected nerves.
Your healthcare team will also consider other conditions that mimic stenosis, like poor circulation, hip arthritis, or peripheral neuropathy. This thorough approach ensures you get the right diagnosis and treatment.
More info about physical therapy clinic back pain
Proven Conservative Treatments
Good news: most people with spinal stenosis symptoms respond beautifully to non-surgical treatments, especially when started early. At Wright Physical Therapy across Idaho and Utah, our approach focuses on evidence-based methods that truly work.
Physical therapy forms the cornerstone of effective treatment. We’ll guide you through gentle flexion-based exercises that create more space in your spinal canal, relieving pressure on pinched nerves. Core strengthening provides better support for your spine, while our hands-on manual therapy techniques help improve mobility and reduce pain.
“I tell my patients to think of their spine like a house with a solid foundation,” says one of our therapists. “When we strengthen your core, we’re reinforcing that foundation, making everything more stable and comfortable.”
Beyond therapy, simple lifestyle adjustments make a huge difference. Low-impact activities like swimming or stationary cycling keep you moving without aggravating symptoms. Weight management reduces stress on your spine, while over-the-counter anti-inflammatories can help manage pain flares. For those needing additional relief, epidural injections may provide temporary comfort while you work on longer-term solutions.
Your physical therapist at Wright Physical Therapy will create a program custom specifically to your needs – one that addresses your unique spinal stenosis symptoms and helps you return to the activities you love.
More info about therapeutic exercise
Emergency Red Flags—Act Now
While most spinal stenosis develops gradually, certain symptoms should send you straight to the emergency room:
Sudden loss of bowel or bladder control isn’t just inconvenient – it’s a medical emergency signaling possible cauda equina syndrome. Similarly, numbness in your “saddle” area (the parts of your body that would touch a saddle when riding a horse) needs immediate attention.
Severe or rapidly progressing weakness in your legs or arms, inability to walk, or sudden, severe pain are all warning signs that something serious is happening. These symptoms might indicate severe compression of your spinal cord or nerve roots that could lead to permanent damage if not addressed quickly.
Trust your instincts. If something feels seriously wrong, don’t wait for your next scheduled appointment – seek emergency care right away. When it comes to your spine, it’s always better to be cautious.
Prevention & Long-Term Outlook
While we can’t stop the clock on aging, we can certainly take steps to keep your spine as healthy as possible for years to come.
Good posture isn’t just about looking confident – it helps maintain proper spinal alignment and reduces unnecessary stress. Regular, gentle exercise keeps supporting muscles strong and flexible. Many of my patients find that maintaining a healthy weight dramatically reduces their symptoms by lightening the load on their spine.
Other helpful habits include avoiding smoking (which accelerates disc degeneration), ensuring adequate calcium and vitamin D intake for bone health, and using proper body mechanics when lifting or carrying items.
The long-term outlook for spinal stenosis varies from person to person. Many of our patients successfully manage their symptoms with conservative care for years or even decades. As one of our physical therapists likes to say, “Your body has an amazing capacity to adapt – we just need to give it the right tools and environment to do so.”
Even for those who eventually need surgery, starting with conservative approaches like physical therapy often improves outcomes. At Wright Physical Therapy, we’re committed to helping you find the least invasive, most effective path to relief from your spinal stenosis symptoms.
Conclusion & Next Steps
Living with spinal stenosis symptoms can be challenging, but recognizing the warning signs early and seeking appropriate care can make a significant difference in your quality of life. Remember these key points:
- Spinal stenosis symptoms vary depending on the location and severity of narrowing
- The classic “shopping cart sign” (relief with forward bending) is a hallmark of lumbar stenosis
- Cervical stenosis can cause more serious symptoms affecting balance and coordination
- Most cases can be managed effectively with conservative care, especially when started early
- Certain red-flag symptoms require emergency attention to prevent permanent nerve damage
At Wright Physical Therapy, our team of specialists across Idaho and Utah locations understands the complex nature of spinal stenosis. We provide personalized physical therapy interventions that target your specific symptoms and functional limitations.
Early evaluation and treatment can prevent further nerve damage and help you maintain your independence and activity level. If you’re experiencing symptoms that might indicate spinal stenosis, consider reaching out to our team for a comprehensive assessment.
Remember: While spinal stenosis is a common age-related condition, its symptoms don’t have to limit your life. With proper diagnosis and management, many people continue to enjoy their favorite activities with minimal limitations.


